Tonsils are small tissue masses at the back of the throat. They help trap germs early in life. Over time, some people develop problems with their tonsils. In those cases, surgery may become a realistic option. A tonsillectomy is the removal of the tonsils through a simple surgical procedure. However, deciding to remove them isn’t always straightforward. Let’s explore the different signs, patterns, and symptoms that might lead someone to this decision.
Tonsillitis that keeps returning every few weeks
Recurring infections often trigger the first serious discussions about tonsillectomy. If someone experiences tonsillitis many times in a short period, doctors take notice. Especially when these episodes happen six or more times in a year. Sometimes the infections go on for years. The pattern usually includes fever, sore throat, and swollen glands. Antibiotics work for a while, but then stop being effective. This ongoing cycle drains energy and interrupts daily life. When conservative treatments fail repeatedly, surgery becomes the next logical step. Patients are usually tired of the pain and disruption. At that point, they’re more open to permanent solutions.
They noticed my tonsils are always swollen and uneven
Not all tonsil problems involve pain or fever. Some people visit their doctor for a different reason. Their tonsils are large all the time, even when there’s no infection. In some cases, one tonsil is much bigger than the other. That asymmetry raises questions. Doctors may suspect a hidden condition. Uneven or constantly enlarged tonsils can sometimes hide something more serious. A biopsy may be ordered to rule out rare diseases. If the appearance doesn’t change over time, removal becomes a safe option. It’s a way to be sure nothing dangerous is growing unnoticed.
My child can’t sleep properly because of loud snoring
Children with sleep issues often have enlarged tonsils. Parents describe loud snoring or gasping during the night. Some children even stop breathing for a few seconds while asleep. This condition is called obstructive sleep apnea. It affects concentration, growth, and mood during the day. In such cases, tonsils are blocking the airway. Removing them makes a huge difference. Most parents report better sleep patterns and daytime behavior after the operation. It’s one of the main reasons children undergo tonsillectomy. Pediatric specialists usually decide based on sleep quality, not just throat infections.
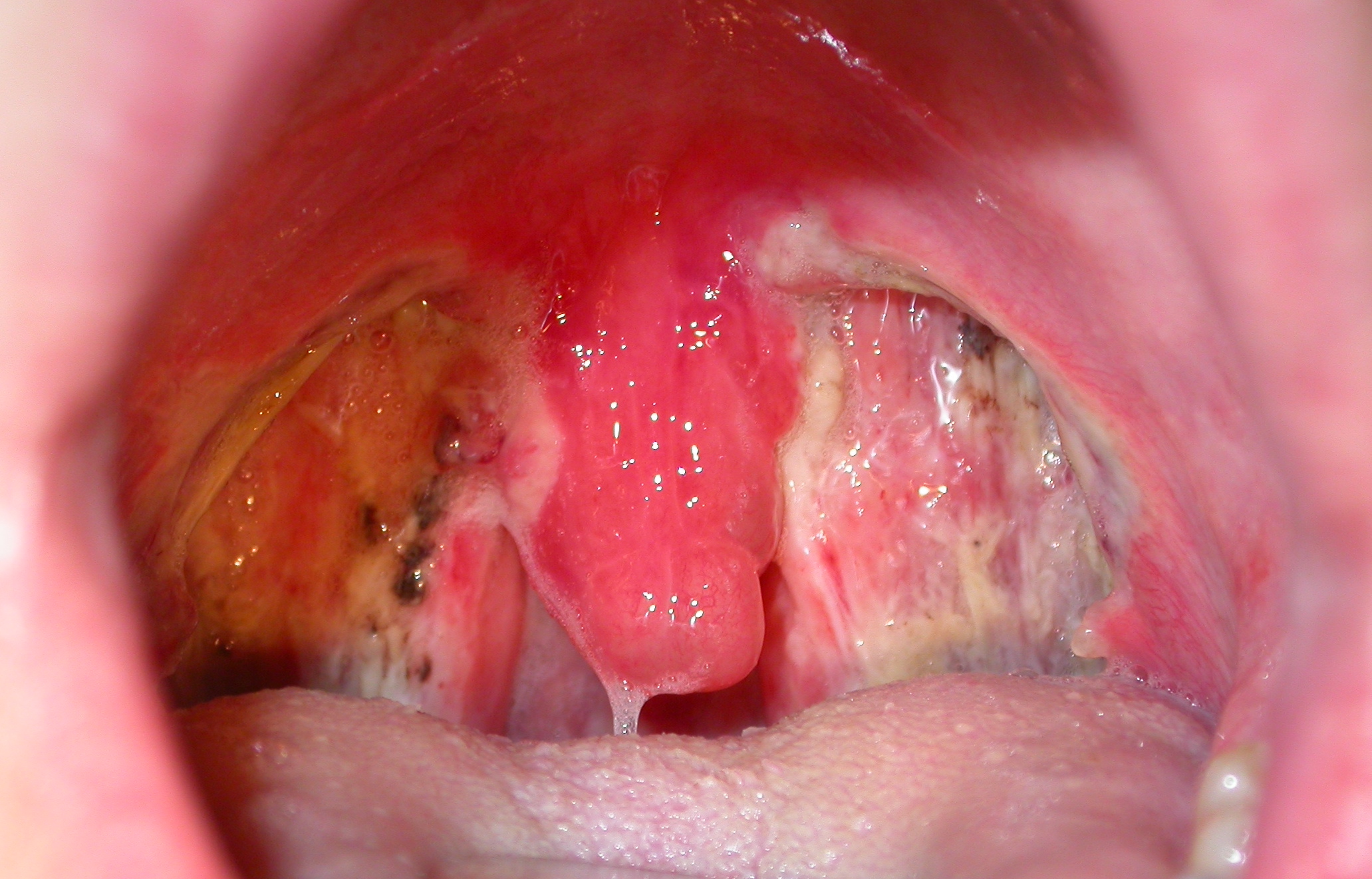
I kept getting peritonsillar abscesses every year
A peritonsillar abscess is more intense than a typical sore throat. It’s a pocket of pus near the tonsils. It often forms after untreated or severe tonsillitis. The pain is usually one-sided and intense. Speaking, swallowing, or even opening the mouth becomes difficult. Doctors first treat it with drainage and antibiotics. But for some patients, the abscess keeps coming back. This recurrence makes long-term solutions necessary. Tonsillectomy helps prevent future infections and complications. For many, it’s the only way to stop the abscess cycle from repeating yearly.
I could barely eat or breathe without feeling pressure
Tonsils sometimes grow so large that they block basic functions. People describe constant pressure while eating or breathing. This can lead to choking sensations, especially at night. Some even feel the tonsils touching in the middle. It’s not always caused by infection. For others, it’s simply their anatomy. In these cases, removing the tonsils allows normal airflow and food passage. The relief is noticeable almost immediately. Patients regain comfort with meals and feel less tired during the day. Quality of life improves significantly with this simple change.
My bad breath wouldn’t go away despite brushing everything
Chronic bad breath isn’t always about hygiene. In some cases, tonsil stones are to blame. These are small, hardened bits of food and bacteria stuck in the tonsils. They create an unpleasant smell and taste. Mouthwash and flossing don’t help much. People often feel like something is stuck in their throat. Tonsil stones can also cause coughing or discomfort when speaking. For those affected regularly, a tonsillectomy is a permanent fix. Once the tonsils are gone, the stones stop forming. Breath improves, and throat irritation disappears.
Antibiotics don’t work like they used to on me
Overuse of antibiotics leads to resistance. After years of treating tonsillitis with pills, many patients notice something. The infections don’t respond as they used to. The recovery takes longer. The symptoms are stronger. Some develop side effects from repeated antibiotic use. Doctors weigh the long-term risks. If the tonsils are the root cause, removing them can end this cycle. It reduces dependence on medication and future health risks. It’s not about giving up. It’s about shifting to a more sustainable solution.
My doctor said the benefits now outweigh the risks
Surgery always has risks. Bleeding, infection, and anesthesia reactions are real possibilities. That’s why doctors don’t rush into tonsillectomy. But when symptoms persist despite all efforts, the balance changes. The pain, the hospital visits, the sleep issues—everything adds up. At a certain point, the burden becomes heavier than the surgery’s risk. That’s when professionals suggest going forward. Every patient is different. Some reach this stage in childhood. Others arrive much later. What matters is recognizing the personal cost of not acting.
I had mono, and my tonsils haven’t been the same since
Infectious mononucleosis, often called mono, can affect the tonsils severely. During the illness, they swell and become painful. For most people, things return to normal. But some continue having problems long after recovery. Their tonsils remain enlarged or become more prone to infections. These long-term effects aren’t always predictable. Doctors monitor for several months before suggesting surgery. If the pattern continues, tonsillectomy becomes part of the conversation. It’s about breaking free from the illness’s lingering shadow.
I’ve been missing school or work too often because of sore throats
Frequent absences hurt more than physical health. They impact school progress and job performance. Employers become frustrated. Students fall behind. A sore throat may seem minor, but not when it happens monthly. Some even end up in urgent care every few weeks. This routine takes a toll on mental health. Patients feel stuck in a cycle they can’t control. If tonsil infections are the main reason, removing them changes everything. Productivity returns. Stability improves. People finally move on from recurring interruptions.
My ENT specialist said this is the right time
ENT doctors see thousands of throats every year. They don’t recommend surgery casually. But when the signs are clear, they know. They look at patterns, not single events. Their judgment often comes after months of tracking symptoms. When they finally suggest a tonsillectomy, it’s rarely a surprise. Most patients have already considered it. What the specialist offers is timing and confidence. Having a professional’s input makes the decision easier. It’s about trusting experience and looking forward to relief.
I didn’t know tonsils could cause this many problems
Many people underestimate their tonsils. Until problems begin, they barely think about them. But for those with chronic issues, the tonsils become a major factor in daily life. Pain, fatigue, embarrassment, even isolation—these symptoms pile up. When nothing else works, tonsillectomy becomes a doorway out. It’s not about chasing perfection. It’s about removing a source of trouble that refuses to go away. Life after the surgery usually feels easier. Not perfect, just less burdened. And sometimes, that’s all a person needs.