Many people notice symptoms beyond sneezing during allergy season. They complain of pressure behind their eyes. Others feel constant fatigue without understanding why. These symptoms are not always from a cold. In many cases, it’s a sinus reaction to allergens. When the nasal lining swells, mucus can’t drain properly. That’s when pain and pressure start building up. Allergy inflammation affects more than just your eyes and throat.
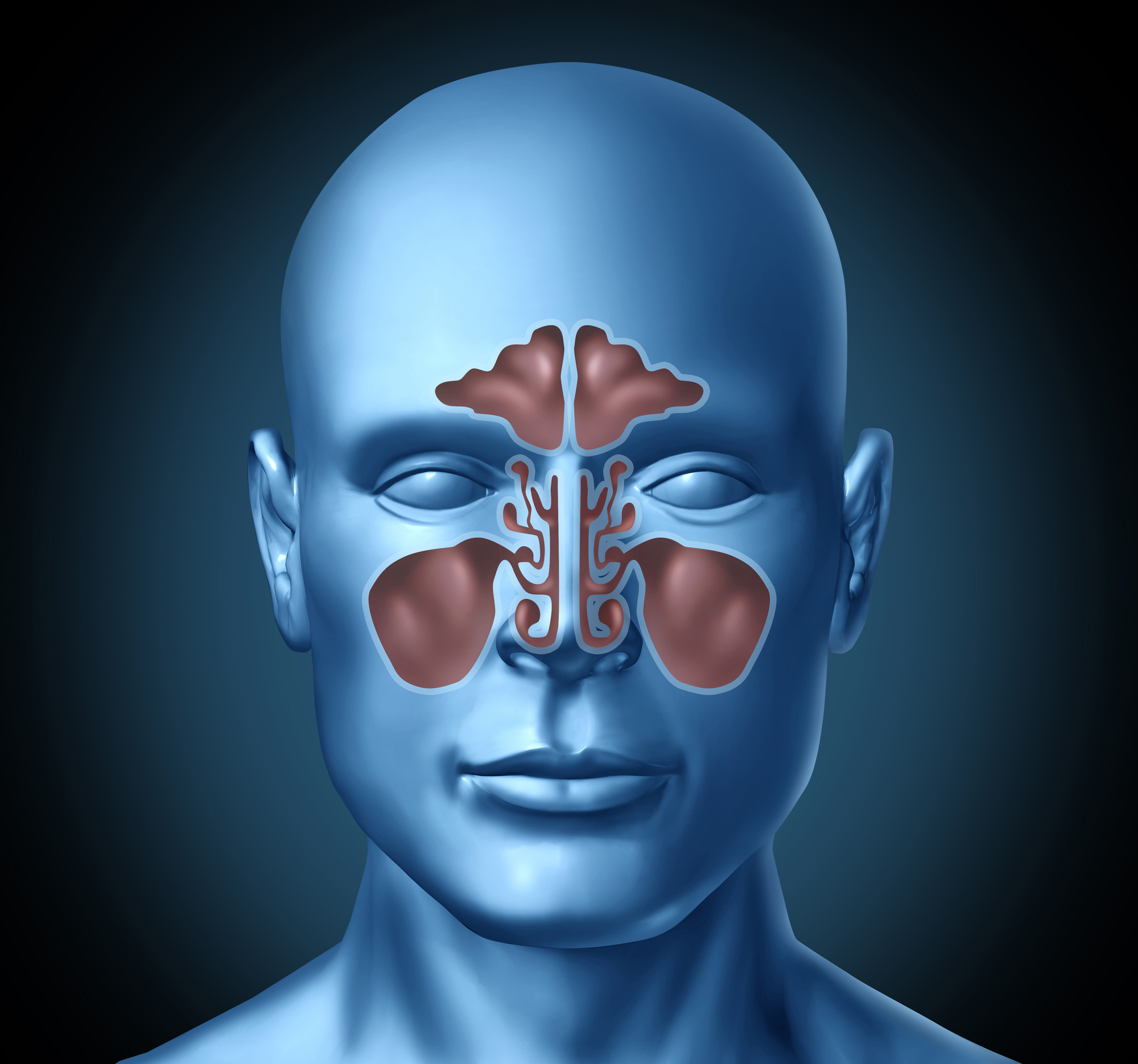
Sinus pressure builds when drainage is blocked
Inside the face, sinus cavities are small air-filled spaces. They need open pathways to drain mucus. When allergens like pollen or dust trigger inflammation, these passages swell shut. The trapped fluid creates a feeling of pressure. Some people describe it as a dull ache. Others say it feels like wearing a heavy helmet. Either way, it often points to an allergic reaction in the background.
Nasal congestion can stem from invisible allergens
Most people associate congestion with a cold. But chronic stuffiness often points to indoor triggers. Dust mites, pet dander, and mold are frequent culprits. These microscopic particles float in the air unnoticed. When inhaled, they provoke an immune response. Over time, the nose becomes blocked every morning. For some, it lasts all day. It’s not just an annoyance—it signals underlying sinus strain.
Not all sinus problems involve infection
People often assume sinus pain means they’re sick. But sinus inflammation isn’t always caused by bacteria. Allergies alone can produce the same swollen tissues and blocked drainage. The difference lies in the mucus. In bacterial cases, it’s often thick and yellow. In allergic rhinitis, it’s usually clear and runny. The discomfort can feel identical, though, leading many to mistreat it.
Chronic sinusitis may begin with allergic rhinitis
Allergic rhinitis causes recurring swelling in nasal tissues. If untreated, this can evolve into chronic sinusitis. The sinuses stay inflamed for weeks or even months. This long-term blockage becomes a breeding ground for secondary infections. But the root issue is often the allergic trigger. Without addressing it, relief remains temporary. Many people ignore this connection and focus only on symptoms.
Inhaled allergens spark reactions in the upper airways
When you breathe in allergens, your immune system reacts quickly. The nose and sinuses become frontline defenders. Histamines are released to flush out irritants. But that response also brings swelling, congestion, and drainage issues. Over time, this reaction trains the body to overreact. Even small exposures can trigger noticeable symptoms. The sinuses suffer the most from this repeated cycle.
Sinus infections are more common in allergy-prone individuals
People with allergies face higher risks of sinus infections. Their nasal passages stay inflamed longer than normal. This ongoing swelling restricts proper drainage. Bacteria find these moist, stagnant spaces perfect for growth. It’s a pattern seen often in clinical studies. One flare-up leads to another, creating a frustrating cycle. Prevention requires more than antibiotics—it involves allergen control.
Misdiagnosis leads to unnecessary treatments
Many sinus issues caused by allergies are misdiagnosed. People take antibiotics when they don’t need them. This not only fails to help but may harm long-term health. Overprescribing antibiotics can lead to resistance and gut imbalance. Doctors now emphasize distinguishing between allergic and infectious causes. A clear diagnosis depends on both history and symptom patterns.
Nasal sprays help, but don’t solve root issues
Corticosteroid sprays reduce swelling in the nasal passages. They’re commonly prescribed for both sinus and allergy symptoms. While they ease discomfort, they don’t eliminate triggers. Relief is temporary unless allergens are controlled. Long-term use of sprays can also irritate tissues. So while helpful in acute phases, they’re part of a broader approach. Allergy management is still the core solution.
Allergy tests reveal the hidden culprits
Many people suffer for years without knowing their exact triggers. Skin and blood tests can uncover specific allergens. These might include pollens, molds, or pet dander. Knowing what you’re sensitive to changes everything. You can adjust your environment and habits more effectively. That’s often the turning point between chronic symptoms and long-term control.
Humidity and air quality affect sinus health
Dry air irritates sinus tissues and worsens congestion. Too much humidity encourages mold growth, another allergy trigger. Finding a balance is essential. In Dubai, air conditioning plays a major role. It cools but can dry out mucous membranes. Humidifiers can help—but overuse invites dust mites. Air purifiers with HEPA filters provide clean, balanced air for sinuses.
Food allergies can influence sinus reactions too
Though less common, certain foods trigger sinus-like symptoms. Dairy, wheat, and soy often come up in elimination diets. These don’t cause congestion like pollen, but they can increase inflammation. Some people find their sinuses clearer after dietary changes. It’s not always about airborne allergens. What we eat shapes our immune responses too.
Sleep quality drops when sinuses are inflamed
Chronic congestion disrupts sleep. People wake up tired, foggy, and irritable. Breathing becomes shallow. Oxygen intake is reduced throughout the night. For children, this can affect growth and behavior. Adults may snore more or develop sleep apnea. Addressing sinus and allergy issues often restores sleep naturally. This benefit is sometimes overlooked but deeply impactful.
Allergy seasons shift with climate change
Warmer winters and longer springs change pollen cycles. Plants bloom earlier and for longer periods. This means allergy season no longer has a clear start or end. Sinus sufferers experience symptoms more unpredictably. Traditional remedies may no longer align with environmental patterns. New strategies must reflect these shifts in exposure.
Not all over-the-counter treatments are harmless
People often self-medicate for sinus pain. Decongestants offer quick relief but cause rebound symptoms. Nasal tissues become dependent, worsening congestion over time. Antihistamines vary in effectiveness and side effects. Drowsiness, dry mouth, or irritability are common. Reading labels and consulting a doctor prevents unintended consequences. Natural doesn’t always mean safe either—some herbal remedies interfere with medications.
Mold exposure can happen in unexpected places
Mold isn’t just a basement problem. It grows behind walls, inside air vents, or under carpets. Dubai’s humid climate increases indoor mold risks despite frequent AC use. Even new buildings aren’t immune. Mold spores can be inhaled without smell or visible signs. Sinus issues may persist despite surface cleanliness. Professional inspections can identify hidden growth.
Children experience allergy-sinus connections differently
Kids often can’t explain sinus pressure clearly. They say their head hurts or feel tired. Chronic mouth breathing and nasal voice are subtle clues. Pediatricians watch for these in allergy-prone children. Left unchecked, this may affect facial development. Enlarged adenoids or ear infections often follow. Early allergy care reduces sinus complications in childhood.
Pets can trigger year-round sinus inflammation
Even short-haired animals produce allergens. Proteins in skin flakes, saliva, and urine cause reactions. These stick to furniture, clothing, and carpets. Vacuuming helps, but can also stir allergens into the air. Air purifiers and strict bedroom boundaries reduce exposure. For allergic individuals, pet ownership requires constant management. The sinuses are often first to show signs of irritation.
Sinus surgery doesn’t cure allergies
Some people pursue surgery after chronic sinus issues. Procedures widen drainage pathways for better airflow. But if allergies remain untreated, problems return. Surgery fixes the plumbing, not the water source. That’s why allergist consultation is often recommended first. Managing inflammation avoids surgical recurrence. It’s a partnership between ENT specialists and allergy doctors.
Travel habits influence sinus health too
Flying dries out sinus membranes. Cabin pressure changes worsen blockages. Hotel rooms may contain unfamiliar allergens. People often report sinus flares after long trips. Using saline sprays during flights helps maintain moisture. Carrying your own pillowcase may reduce exposure. Planning ahead eases transitions for sensitive sinuses.